Introduction to Urinary Retention
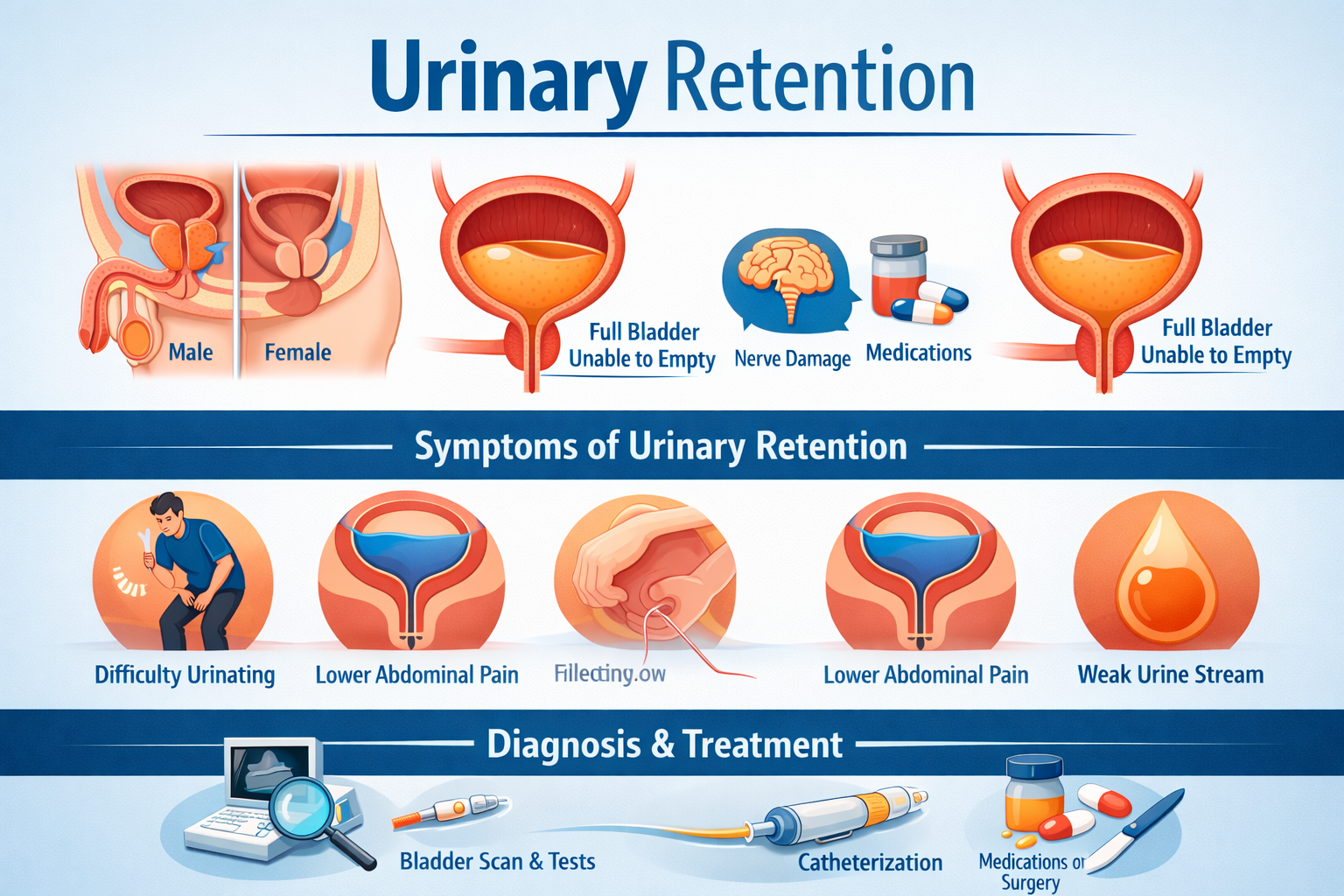
Urinary retention is a condition characterized by the inability to empty the bladder completely or at all. It can develop suddenly or evolve gradually over time. When untreated, it may lead to discomfort, infection, and progressive damage to the urinary system.
Two primary forms exist. Acute urinary retention occurs abruptly and constitutes a medical emergency. Chronic urinary retention develops insidiously, often remaining unnoticed until complications arise. Both forms demand clinical attention.
How Normal Urination Works
Normal urination is a finely orchestrated physiological process. The bladder stores urine while remaining relaxed. When fullness is achieved, sensory nerves transmit signals to the brain, initiating the voiding reflex.
Simultaneously, the detrusor muscle contracts as the urinary sphincters relax. This coordination allows urine to flow freely. Any disruption in this neuromuscular dialogue can impair bladder emptying and result in urinary retention.
Common Causes of Urinary Retention
Obstruction is among the most frequent causes. In men, an enlarged prostate can compress the urethra, restricting urine flow. Urethral strictures, bladder stones, and tumors may also physically impede emptying, The inability to urinate or empty your bladder completely.
Neurological causes are equally significant. Conditions such as spinal cord injury, multiple sclerosis, diabetic neuropathy, and stroke can interfere with nerve signals between the bladder and brain. When communication fails, bladder contraction becomes ineffective.
Certain medications contribute to urinary retention by altering muscle tone or nerve signaling. Antihistamines, antidepressants, anticholinergics, and opioid analgesics are common culprits. Postoperative urinary retention may also occur due to anesthesia and temporary nerve suppression.
Risk Factors and Vulnerable Populations
Advancing age is a notable risk factor, particularly among men due to prostate enlargement. Women may experience urinary retention following pelvic surgery or childbirth-related trauma.
Chronic illnesses such as diabetes, Parkinson’s disease, and kidney disorders increase vulnerability. Reduced mobility, dehydration, and recurrent urinary tract infections further exacerbate risk.
Symptoms and Warning Signs
Symptoms vary depending on severity and duration. Early signs include weak urine stream, difficulty initiating urination, and a sensation of incomplete emptying. Increased urinary frequency with minimal output is also common, Urinary retention.
In more advanced cases, lower abdominal pain, visible bladder distension, and overflow incontinence may occur. Untreated urinary retention can lead to recurrent infections, bladder damage, and impaired kidney function.
Diagnostic Evaluation
Diagnosis begins with a detailed medical history and physical examination. Palpation or percussion of the lower abdomen may reveal bladder distension. In men, prostate evaluation is essential.
Bladder ultrasound or post-void residual volume measurement confirms incomplete emptying. Additional investigations may include urine analysis, blood tests for kidney function, cystoscopy, or urodynamic studies, depending on suspected cause.
Treatment Options for Urinary Retention
Immediate relief often involves catheterization to drain retained urine and prevent complications. This intervention rapidly alleviates discomfort and protects renal function.
Medical management targets the underlying cause. Alpha-blockers may relax the bladder neck and prostate muscles. Antibiotics are prescribed if infection is present. Medication adjustments may be necessary when drugs contribute to retention.
Surgical or procedural interventions are considered when conservative measures fail. These may include prostate surgery, urethral dilation, or correction of anatomical abnormalities. Neuromodulation techniques may benefit select neurological cases.
Long-Term Management and Prevention
Long-term care focuses on preventing recurrence and preserving urinary tract health. Adequate hydration, bladder training exercises, and scheduled voiding can improve bladder efficiency.
Regular follow-up is crucial, particularly for individuals with chronic conditions. Early detection of changes allows timely intervention and reduces the risk of complications.






Leave a Reply